
By Tom Peterson
Helping Americans move to better health seems like an impossible, quixotic dream. But it is possible. And because of their unique size and role, health systems could hold the key. The more than 5,000 hospitals have a combined budget of $3.8 trillion. Combined they are country’s second largest private employer and individually are often the largest employer in their community. While they mostly focus on medical solutions to specific illnesses, a growing number of hospitals are venturing outside their walls to improve health, wellness and quality of life of their communities.
When it comes to radically improving health, hospitals could act as giant change agents. And this movement is already started.
The Child Survival Campaign
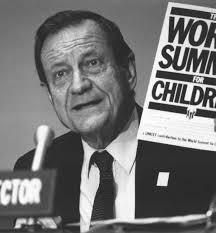
The Child Survival Campaign, launched by Unicef’s James Grant in the 1982 State of the World’s Children, was touted as a “revolution.” Grant (pictured below) identified four practices that when put into place could radically reduce deaths and improve child health. Campaigns were rolled out to vaccinate against six childhood diseases, track children’s weight, encourage breast feeding and use oral rehydration therapy when needed. Believed to be game changers, these four efforts were deployed globally on an unprecedented scale.
 The practices and principles were constant, but they played out quite differently from country to country and even within the nations. In some places the bishop or imam’s word made the difference. Governments, nongovernmental agencies, faith institutions, schools, the media and others joined the effort. Rotary International stepped up to the challenge of eradicating polio. The Herculean efforts took place amidst poverty, corruption and every other imaginable hurdle. From the UN headquarters to a Salvadoran village, people doggedly pushed forward. Wars were even temporarily stopped so children could be immunized.
The practices and principles were constant, but they played out quite differently from country to country and even within the nations. In some places the bishop or imam’s word made the difference. Governments, nongovernmental agencies, faith institutions, schools, the media and others joined the effort. Rotary International stepped up to the challenge of eradicating polio. The Herculean efforts took place amidst poverty, corruption and every other imaginable hurdle. From the UN headquarters to a Salvadoran village, people doggedly pushed forward. Wars were even temporarily stopped so children could be immunized.
So how did it go? Here’s how Nicolas Kristoff describes it in a 2008 column in the New York Times:
The number of children who die worldwide each year before the age of five has dropped below 10 million for the first time in recorded history—compared with 20 million annually in 1960—Unicef noted in a report last month, “Child Survival.” Now the goal is to cut the death toll to four million by 2015.
Think about that accomplishment: The lives of 10 million children saved each year, 100 million lives per decade.
To put it another way, the late James P. Grant, a little-known American aid worker who headed Unicef from 1980 to 1995 and launched the child survival revolution with vaccinations and diarrhea treatments, probably saved more lives than were destroyed by Hitler, Mao and Stalin combined.
An estimated 5.9 million children under age five died in 2015. The goal of cutting it to 4 million was missed, but it’s still giant progress from the 20 million who died in 1960.
Journey of Health
 U.S. health challenges are often seen as too complex and entrenched to be fixed. Protecting their self-interests, powerful industries may impede progress. The health of individuals and whole populations is tied to so many other “social determinants.” Yet these systems are no more complex than the world’s almost 200 countries, each with their cultures, governments and religions. If the child survival campaign and following efforts could cut both the rate and number of child deaths by more than half, surely, we can bring health and wellness to the world’s wealthiest nation.
U.S. health challenges are often seen as too complex and entrenched to be fixed. Protecting their self-interests, powerful industries may impede progress. The health of individuals and whole populations is tied to so many other “social determinants.” Yet these systems are no more complex than the world’s almost 200 countries, each with their cultures, governments and religions. If the child survival campaign and following efforts could cut both the rate and number of child deaths by more than half, surely, we can bring health and wellness to the world’s wealthiest nation.
Health systems are teeming with staff who chose their careers because they wanted to help others. Too often they can only wait inside their walls for the really sick to come in the door, often through the emergency room. The sickest are then treated and released back to their lives outside. To be fair, that’s what hospitals were generally designed to do. Inside the walls people are often cured and lives are saved.
But a person’s health journey takes place mostly outside the hospital walls. And in the emerging model, many hospitals are partnering with local businesses, schools, public health departments, nonprofits and other organizations to focus resources on the community where these sometime patients live most of the time.
 They are trying to understand how to best engage with the most vulnerable people. They are sharing not just what programs work, but also what deeper principles undergird the programs that make them succeed. U.S.hospitals have a talent pool that is historically unprecedented, with it’s sheer size, amazing talent and motivation to bring about health.
They are trying to understand how to best engage with the most vulnerable people. They are sharing not just what programs work, but also what deeper principles undergird the programs that make them succeed. U.S.hospitals have a talent pool that is historically unprecedented, with it’s sheer size, amazing talent and motivation to bring about health.
Jonas Salk asked, “What must we do to evoke the greatest potential from ourselves and from others?” It’s a question every health system should ask about itself and its community. Many hospitals are stepping up and, as in the early years of the Child Survival campaign, they’re already seeing some early wins.
Photo: James Grant, Unicef.org. Art: Andreas Bogdain, Creative Commons.
Hospitals are keystone species in an ecological system of care that are part of every community in which they reside. This has always been the case although because of the payment and reimbursement system this was not self-evident. Now with imperatives of population health and health equity, it necessary that hospitals (especially Stakeholder Health hospital) begin to understand it particular and important role a top of the food change. Everything in does has an impact of what as been termed the Social Determinants of Health (SDOH). These SDOH include employment, housing, education, builded environment, public policy and so on. The greatest opportunity the Stakeholder Hospital have to be change agents is to be mindful of everything it does impact SDOH. One organization that has been mindful of the thesis Kaiser Permanente. It has begun to target it purchasing power, building decisions, employment practices, political influence proactively to change the health of communities through its strategic investments. What if every hospital begun to take similar approach to its business practices.
With new emphasis on Population Health and Health Equity, it become increasing important that Hospital understand that it must transform itself from a closed system that in internally focused to an open system that is fully connectable to its community. To be a Health System that is ecologically responsible, it must me a connectable to that ecology. This mean the Hospital in with begin to perceive itself as apart of an integrated community-based Health System rather than the Big Box on the hill. This has been the approach of the Wake Forest Baptist Medical Center FaithHealth Division with it Supports of Health who are form EVS worker turned community health workers. It is best expressed by what has been referred to the as the Memphis Model which is some 600 congregation, nine FQC faith-based community clinic, a variety on community based social services agencies tied together by Navigators employed by Methodist Lebonhuer Health System.
By strategically using its keystone role in the community ecology by becoming a connectable open system hospital can truly be come a change agent. The way wolves can change the course of a river, hospitals can change the course of the social determinants of health.