
By Tom Peterson
Inspired in 2002 by frequent blackouts, Brazilian mechanic Alfredo Moser (pictured) thought up a simple technology that’s literally a brilliant idea. Just fill a clear plastic soda bottle with water (add bleach to prevent algae clouding), cut a hole in the roof of the house and snugly place the bottle in the hole so the rain won’t get in. It takes less than an hour to make and install. And behold: the sunlight brightens the room as though it were a 50-watt bulb. Of course, it shines only during the day.
Moser’s idea slowly spread, and in 2011, news articles and viral videos about the solar bulbs suddenly increased awareness about his concept. They described how to make the lights and the unique ways that they were being used around the world. One group in the Philippines was installing 140,000 lights in slums across the country. Today these simple bulbs brighten once dark rooms for millions in Kenya, Peru, Mexico, India and many other countries. Entrepreneurs are even turning bulb making and installation into small businesses.
What is more powerful than the spread of a practice that improves life? And what is more wasteful than a great solution doesn’t spread? But how do good ideas spread?
Scaling up through the spread of ideas
 Stakeholder Health is about spreading ideas and practices. It’s also about how we view the world and our role in it. It’s about health systems and the communities they serve learning together and sharing ideas that work—from one hospital and one community to another. Done well, we help improve the health of our most vulnerable citizens.
Stakeholder Health is about spreading ideas and practices. It’s also about how we view the world and our role in it. It’s about health systems and the communities they serve learning together and sharing ideas that work—from one hospital and one community to another. Done well, we help improve the health of our most vulnerable citizens.
How does an improvement—a new practice or great tweak on an existing one—move from one system and go to scale? Being part of the Stakeholder tribe means we have the trust and the generosity to share deeply—not just the nuts and bolts of a practice, but also the deeper nuances of why a practice works in this place, what failed, and what we’re still trying to figure out. It means, too, that we are willing to learn from others and to ask for help.
What it takes to spread practices
Nicole Dubbs and Kerry Anne McGeary, were curious about how social change ideas spread. With the Robert Wood Johnson Foundation and the Monitor Institute they spent six months exploring with creative people and experts “what it takes to spread ideas that others adopt, adapt, integrate, and ultimately take up as their own.” They share four conclusions in the Stanford Social Innovation Review. And their findings speak directly to the work of Stakeholder Health partners:
- Where you intervene in a system is important.
- Stakeholders don’t act on abstract ideas.
- Moving away from a traditional program focus is useful.
- Shape the rhetoric and shift action.
Stakeholder Health intervenes in two key spheres: within a hospital itself and in the surrounding community outside of the hospital’s walls. Usually, somewhere within a health system, a handful of committed people are already reaching into their community. A few of these are strategically located (often one reports directly to the CEO), their jobs are relevant to improving the health of their community’s most vulnerable residents, and they have passion or “heart.”
 They are realigning resources of the hospital with those of the community in a way that improves health of the most vulnerable. How each group moves forward within their own system and community depends on their local context. And along the way they share what they have learned, adding to the collective knowledge of the tribe.
They are realigning resources of the hospital with those of the community in a way that improves health of the most vulnerable. How each group moves forward within their own system and community depends on their local context. And along the way they share what they have learned, adding to the collective knowledge of the tribe.
So where within a community does the health system intervene? That depends, because each situation is different. When the hospital truly listens to the community, the correct actions will present themselves. Mapping exercises in the Hispanic community in Winston-Salem, North Carolina, resulted in the need to focus on getting identification cards for undocumented residents so they are able to get prescriptions and drive to a medical appointment without fear of being deported. In Toledo, Ohio, Promedica heard the need for a grocery store to bring healthy food to a food desert. Advocate Health Care in Chicago heard about ways to stop violence. In San Francisco, Dignity Health heard a need for below-market loans for nonprofits working towards improving the community. Bon Secours Baltimore heard a need for decent housing. These and other health systems hear the challenges and, alongside their community partners, take action.
Community Benefits requirements of the Affordable Care Act are not the point. Rather, how does a hospital align its own resources and assets with those of its community in true partnership to improve health for the most vulnerable? Participating health systems now use phrases such as hotspotting, navigation networks or congregational health networks, health asset mapping, strategic investment, leading causes of life, outside the walls to describe their initiatives. These phrases and others inform actions and are translated into partnerships doing real-life work.
Adapted not replicated
From the outset, the Stakeholder community has shied away from the notion that a practice such as a congregational health network can be “replicated.” (Although using the categories of van Oudenhoven and Wazir (see below) most Stakeholder sharing would fall somewhere between “concept” and “spontaneous” replication.) These practices are really adapted as they move from one place to another. Hospitals are found in a place and each place has unique challenges and assets. A practice may move from Denver to Atlanta, but it would end up looking quite different because the health systems are different. So are the internal champions, the external partner organizations, the culture, the politics and many other variables. The practice can’t be replicated, but it can be borrowed and adapted.
 These practices can’t mechanically “plug and play” into a new setting. To adapt a program that works in one hospital means understanding foundational principles (see Stakeholder Way). It means having heart for and commitment to the community and being willing to partner with others. This means being transparent and authentic, building trust, and being in a true relationship with the community. However, these are not the main drivers of most health system decisions.
These practices can’t mechanically “plug and play” into a new setting. To adapt a program that works in one hospital means understanding foundational principles (see Stakeholder Way). It means having heart for and commitment to the community and being willing to partner with others. This means being transparent and authentic, building trust, and being in a true relationship with the community. However, these are not the main drivers of most health system decisions.
How can we improve the chances that proven solutions will spread? The starting point has to be when people working on similar challenges pass their stories on to others. They share things that work and their hopes for the next phase, sometimes deeply, through webinars, data-filled PowerPoints, blog posts, and in conversations over lunch or on the phone. The result: spreading of practices and programs that work.
This, it turns out, creates momentum for large-scale change.
Spread Practices Links
9 Ways to Solve Social Problems by Spreading Ideas That Already Work. By Jeffrey Bradach and Abe Grindle
Six Steps to Successfully Scale Impact in the Nonprofit Sector. By Erin Harris
A Smart Way for Philanthropy Ideas to Spread Fast: Change Social Norm. By Howard Husock
BONUS! Five paths to spreading social programs
How do ideas spread? Nico van Oudenhoven & Rekha Wazir described five different paths for replicating social programs in a paper for UNESCO. The paper is worth reading in its entirety, but here’s a summary of their paths:
- Franchise Approach. With a central agency that provides “technical assistance, marketing, training and other services” in a “cookie-cutter” way. The rules are fixed, can’t be changed.
- Mandated Replication. Program is mandated top-down, usually from a government. No choice in how the program works.
- Staged Replication. Three stages: 1) Pilot, the concept is tested; 2) Demonstration, the program is tried in a variety of settings; and 3) Rollout, go to scale.
- Concept Replication. Focus is on not the specifics of the prototype program but on the components and principles that made it work. These are then adapted to fit the local context.
- Spontaneous Replication. Program spreads by “spontaneous and informal contacts between like-minded individuals.” Communication is “a two-way process of convergence where participants ‘create and share information.’”
Which of these make sense for the spread of practices that will improve the health of our communities? There’s no right answer. Many successes will be a mix of at least two of these.
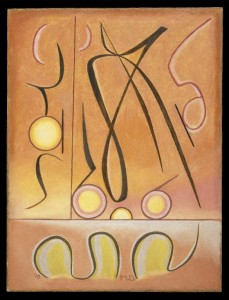
Art: Alfredo Moser, Liter of Light. Painting Manierre Dawson, Brooklyn Museum, Creative Commons.
0 Comments
Trackbacks/Pingbacks